Food addiction differs markedly from regular cravings in both intensity and impact on daily life. While cravings are temporary urges you can typically manage, food addiction involves persistent, compulsive eating patterns that disrupt your normal functioning. You’ll experience loss of control, withdrawal symptoms, and continued consumption despite negative health consequences. True addiction requires meeting specific diagnostic criteria, including tolerance development and failed attempts to quit. Understanding these distinctions can help you identify whether professional intervention might be necessary.
The Science Behind Food Addiction
While the term “food addiction” may sound contradictory given our biological need to eat, scientific evidence reveals striking similarities between compulsive eating patterns and substance use disorders.
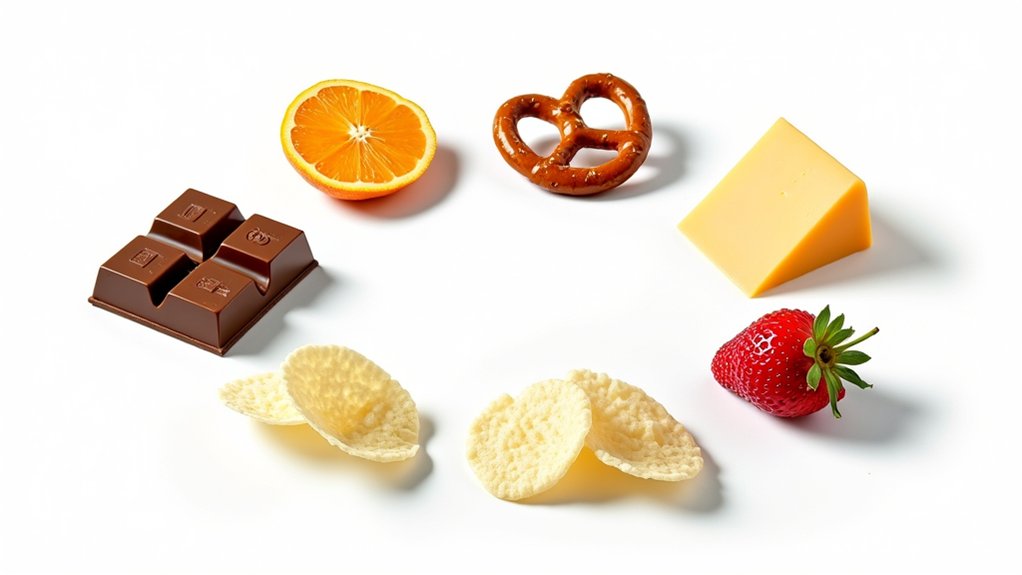
When you consume ultra-processed foods, your brain’s dopamine pathways respond similarly to drug use, creating a reward system that drives continued consumption. This neurobiological process involves changes in your brain’s structure and function, particularly in areas controlling reward and decision-making. Research shows that emotional dysregulation plays an essential role, as your prefrontal cortex’s ability to regulate impulses becomes impaired. The mesolimbic dopamine system becomes sensitized through repeated exposure, leading to pathological behaviors. Studies demonstrate that naturally occurring foods rarely trigger these addictive responses. Food manufacturers specifically design processed foods to reach a bliss point to enhance their addictive potential.
Your genetic makeup can increase susceptibility to food addiction through variations in dopamine receptor genes, while brain-gut-microbiome interactions and hormonal imbalances further contribute to addictive-like eating behaviors. These neurobiological mechanisms create a complex web of factors that distinguish food addiction from regular hunger or cravings.
Key Differences Between Cravings and Addiction
Although many people casually describe their desire for certain foods as an “addiction,” significant differences exist between typical food cravings and clinical food addiction. While craving triggers might include occasional stress or hunger, addiction involves persistent patterns requiring at least two diagnostic criteria, including tolerance, withdrawal, and life impairment. Research shows that nearly twenty percent of adults meet the criteria for food addiction according to the Yale Food Addiction Scale.
You’ll notice that cravings typically remain manageable and temporary, whereas addiction manifests as a loss of control despite negative consequences. Similar to how security measures protect websites from harmful activity, the body has natural mechanisms to regulate normal food cravings. Ultra-processed foods can trigger addictive-like eating behaviors that override these natural mechanisms. In addiction, you’ll experience escalating consumption needs and may withdraw from social activities to eat privately. The distinction becomes clearer when examining frequency: cravings are sporadic and controllable, but addiction involves regular, compulsive behaviors that disrupt daily functioning. Unlike typical cravings, addiction criteria also include failed attempts to quit and continued use despite health consequences.
Warning Signs of Problematic Eating Patterns

Recognizing the warning signs of problematic eating patterns can help differentiate between normal dietary habits and potential food addiction. Watch for these critical indicators that may signal a developing issue:
- You experience loss of control when consuming certain foods, eating past fullness despite physical discomfort, and find yourself unable to limit portions despite repeated attempts. Approximately 14-20% of adults struggle with addiction to ultra-processed foods, making this a widespread concern.
- Your eating habits are driven by emotional triggers rather than hunger, often using food to cope with stress or anxiety, accompanied by feelings of shame or guilt afterward. Genetic predisposition and family eating habits can increase vulnerability to these emotional eating patterns.
- You display compulsive behaviors around food, including secretive eating, preoccupation with obtaining specific foods, and neglecting responsibilities to engage in eating episodes
Physical withdrawal symptoms like headaches and nausea may occur when attempting to avoid trigger foods. These warning signs, when combined with negative consequences in your physical health and social relationships, warrant professional evaluation and support.
Breaking the Cycle: Evidence-Based Solutions
Breaking free from food addiction requires a multi-faceted approach backed by scientific evidence and clinical research. You’ll find the most success through a combination of behavioral techniques, therapeutic interventions, and dietary strategies. When seeking support, 12-step programs offer free, accessible community-based assistance worldwide. Dopamine release during eating reinforces addictive patterns similar to substance use disorders. Addressing emotional distress through proper therapeutic support is crucial, as many individuals turn to food for self-soothing.
| Treatment Approach | Key Benefits |
|---|---|
| CBT Sessions | Restructures thought patterns, identifies triggers |
| Nutritional Education | Stabilizes blood sugar, reduces cravings |
| Structured Meal Plans | Provides portion control framework |
| Professional Support | Guarantees accountability, specialized guidance |
Your recovery journey should integrate evidence-based treatments like Cognitive-Behavioral Therapy with thorough nutritional education. These interventions work together to address both psychological and physiological aspects of food addiction. While some individuals benefit from residential treatment programs, others may achieve success through outpatient care combined with lifestyle modifications and regular therapeutic support. The key lies in selecting interventions that match your specific needs and circumstances.
Building a Healthy Relationship With Food

A healthy relationship with food forms the cornerstone of long-term recovery from food addiction. By embracing intuitive eating principles and developing emotional resilience, you’ll learn to trust your body’s natural hunger signals rather than following rigid dietary rules. Research shows that 45 million Americans attempt dieting annually with poor long-term success rates. Studies indicate that home cooking leads to healthier eating habits, with 30% of daily home cooks reporting very healthy diets. The hypothalamus regulates natural hunger cues, but emotional eating patterns can disrupt these signals.
Key steps to transform your relationship with food include:
- Practice mindful eating by slowing down, savoring each bite, and tracking your body’s responses
- Replace guilt and shame with self-compassion, viewing food as nourishment rather than a moral choice
- Establish consistent meal patterns to stabilize hunger hormones and reduce impulsive eating
This evidence-based approach helps you break free from society’s restrictive food norms while building sustainable habits. Through regular self-monitoring and professional support when needed, you’ll develop the tools to maintain balanced eating patterns without falling into cycles of restriction or compulsion.
Frequently Asked Questions
Can Certain Medications Trigger or Worsen Food Addiction Symptoms?
Yes, certain medications can greatly impact your eating patterns and potentially worsen food addiction symptoms. You’ll find that some antidepressants and mood stabilizers may increase cravings, while withdrawal symptoms from stimulants can trigger compensatory overeating. Additionally, medications affecting your brain’s reward pathways might heighten your response to highly palatable foods. It’s essential to monitor these medication impacts closely with your healthcare provider to adjust treatment as needed.
How Long Does It Typically Take to Overcome Food Addiction?
You’ll typically need to approach food addiction recovery as a long-term journey, with timelines similar to other chronic conditions. Research shows recovery progresses through distinct phases over several years, not weeks or months. While initial improvements can occur within 3-6 months, sustainable recovery often requires 1-2 years of consistent support strategies. Your success rate improves markedly with structured programs, peer support networks, and professional guidance throughout this extended timeline.
Are Some Ethnic Cuisines More Likely to Trigger Food Addiction?
While no ethnic cuisine is inherently more addictive, the way certain dishes are prepared and consumed can influence addiction risk. You’ll find that heavily processed versions of traditional foods, particularly those combining fats and refined carbs, are more likely to trigger addictive responses. Comfort foods and spicy foods across cultures can become problematic when they’re modified to be hyperpalatable through added sugars, fats, and artificial ingredients. The issue lies in modernization rather than traditional preparation methods.
Does Childhood Trauma Increase Susceptibility to Developing Food Addiction?
Yes, your childhood experiences greatly increase your risk of developing food addiction, particularly if you’ve endured severe physical or sexual abuse. Research shows that traumatic experiences can double your susceptibility, with combined abuse forms raising the risk by 2.4 times. Your trauma responses may manifest as using food to cope with negative emotions, and you’re more likely to develop uncontrolled eating patterns. These effects are especially pronounced when trauma spans both childhood and adolescence.
Can Food Addiction Be Passed Down Genetically From Parents to Children?
While research suggests a genetic predisposition to food addiction can be inherited, the exact heritability patterns aren’t fully established yet. You’re more likely to develop food addiction if you have a family history of addiction or eating disorders, as shared genetic pathways involving dopamine signaling may influence your eating behaviors. However, it is essential to recognize that your genes aren’t your destiny; environmental factors play a significant role in whether these genetic vulnerabilities manifest.