Alcohol cravings stem from your brain’s complex neurobiological responses to specific triggers. When you encounter environmental cues, your amygdala activates while heightened ghrelin levels intensify urges. Anxiety and stress increase cortisol, creating a self-reinforcing cycle through disrupted neurotransmitter systems (dopamine, GABA, NMDA). Your psychological state, social pressures, and physical dependencies all contribute to the three-stage addiction loop. Understanding these precise mechanisms reveals effective, evidence-based pathways for managing cravings.
The Brain’s Response to Environmental Cues

When examining the brain’s response to environmental cues in alcohol addiction, the amygdala plays a central role in processing and storing alcohol-related triggers. Your basolateral amygdala shows heightened brain activation when you’re exposed to alcohol-associated scents, particularly during withdrawal phases. Research suggests that ghrelin levels can influence how intensely these environmental triggers affect cravings. Experiments demonstrated that specific scents like anise and orange were used to train rats in associating odors with alcohol presence.
Environmental conditioning becomes more intense during withdrawal periods, as your brain forms stronger neurobiological associations with triggers than during non-dependent phases. You’ll find that cues learned during withdrawal actually override older drinking associations from pre-dependency. This explains why you might experience more intense cravings from triggers encountered during withdrawal states. Research shows that your brain’s response to contextual cues, like specific locations or social settings, creates lasting neural pathways that can persist long after drinking cessation. The study demonstrated that rats in withdrawal showed twice the lever-pressing behavior compared to their pre-dependent state, highlighting the intensified nature of cravings during this phase.
How Emotions and Psychology Drive Cravings
Your anxiety directly influences alcohol cravings, with research showing the highest mean intensity ratings (*M* = 1.44) among emotional triggers. You’ll experience heightened urges during periods of psychological distress, as your brain’s stress response systems become hyperactivated and seek relief through familiar coping mechanisms. Social pressure and peers can intensify these urges significantly, especially in environments like bars or parties. Individuals experiencing high tolerance tend to develop stronger cravings due to their body’s increased dependence on alcohol. Your past trauma can establish persistent drinking patterns, where alcohol becomes neurologically linked to emotional regulation, creating a cycle that requires clinical intervention to disrupt. These patterns are further reinforced when individuals use alcohol as a coping mechanism for emotional pain and stress.
Anxiety Fuels Urge Intensity
Although anxiety and alcohol cravings may appear as separate challenges, they’re intimately connected through complex neurobiological mechanisms. When you experience anxiety, your brain’s emotional regulation centers become hyperactive, triggering intense urges for alcohol. Research shows this connection is particularly strong in individuals with high anxiety sensitivity. Understanding that biological urges can suddenly intensify helps explain the unpredictable nature of cravings.
Your brain’s stress response compounds this effect, as cortisol release combines with anxiety to disrupt dopamine systems and weaken prefrontal cortex control. The statistics reveal the scope: 35.8% of alcohol-dependent men and 60.7% of women have concurrent anxiety disorders. Environmental triggers like work stress or social situations can activate this anxiety-craving cycle. Your brain’s conditioned response to these triggers, coupled with compromised emotional regulation, creates a self-reinforcing pattern that intensifies both anxiety and alcohol urges. Modern treatment approaches like Virtual Reality Cue-Exposure Therapy help break this cycle by systematically desensitizing patients to anxiety-inducing alcohol-related triggers.
Trauma-Triggered Drinking Patterns
Trauma’s impact on alcohol cravings extends far beyond simple cause-and-effect relationships, creating complex neurobiological and psychological pathways that drive compulsive drinking patterns. Research shows that negative emotions mediate the relationship between trauma exposure and alcohol cravings.
Your risk of developing alcohol use disorder increases fourfold if you’ve experienced PTSD, with trauma exposure directly correlating to more severe substance abuse patterns. You’ll find that emotional dysregulation creates a self-perpetuating cycle: alcohol temporarily relieves trauma symptoms but ultimately intensifies long-term psychological distress. The cycle often begins with childhood trauma experiences, which significantly increase vulnerability to developing alcohol dependence later in life. Many individuals turn to alcohol as a form of self-medication, attempting to numb distressing symptoms and painful flashbacks. Environmental cues and stressful situations can unconsciously trigger your alcohol cravings through established neural pathways, even after receiving PTSD treatment.
When you encounter location-based triggers or sensory reminders connected to past trauma, your brain automatically activates craving responses. This mechanism explains why 40% of individuals with substance abuse issues experience concurrent PTSD symptoms, necessitating integrated treatment approaches.
Social Pressures and Cultural Influences

While social drinking appears deeply woven into modern society’s fabric, research shows that peer pressure considerably impacts alcohol consumption patterns across age groups. You’ll face the strongest peer influence between ages 18-34, with 69% reporting pressure to drink, compared to 54-56% in older demographics. These cultural expectations create a complex web of social triggers, where alcohol becomes intrinsically linked to group acceptance and bonding. Mediterranean cultures demonstrate how wine at meals has traditionally enhanced social interactions without promoting excessive consumption. Understanding these triggers helps experts implement security measures to protect vulnerable individuals from harmful drinking patterns.
Digital environments amplify this pressure, as social media normalizes excessive drinking behaviors and reinforces context-dependent cravings. You’re likely to experience stronger urges in specific settings like bars or parties, where group dynamics intensify drinking patterns. The psychological need to belong drives these behaviors, with approximately two-thirds of individuals later regretting alcohol consumption driven by social pressure. Many individuals actively choose to drive to avoid drinking as a strategic way to resist peer pressure while maintaining social connections.
Physical Dependencies and Biological Factors
Beyond social influences, alcohol cravings stem from complex neurobiological mechanisms that fundamentally alter your brain’s structure and function. The chronic consumption of alcohol disrupts your neurotransmitter imbalances, particularly affecting dopamine, GABA, and NMDA systems. These changes impair your reward processing and increase impulsivity.
Your body’s hormonal influences further amplify cravings through multiple pathways. Increased cortisol levels strengthen the connection between stress and alcohol-seeking behavior, while ghrelin fluctuations link hunger with drinking urges. During withdrawal, your brain experiences heightened NMDA receptor activity and glutamate release, triggering intense cravings and potential neurotoxicity. These biological adaptations create a self-reinforcing cycle where your brain’s reward circuits, stress response systems, and decision-making centers become increasingly dysregulated, making resistance to cravings progressively more challenging.
Understanding the Three-Stage Addiction Loop

The addiction cycle operates through three distinct neurobiological stages that perpetuate alcohol-seeking behavior. You’ll experience a complex interplay of brain regions that drive compulsive drinking patterns through neurobiological mechanisms. Your nucleus accumbens initiates the binge stage, while your amygdala controls withdrawal responses, and your prefrontal cortex governs anticipation behaviors. Best treatment practices can help interrupt this cycle effectively. Each stage becomes progressively more intense as habit formation develops through repeated activation of the basal ganglia.
| Stage | Primary Function |
|---|---|
| Binge/Intoxication | Dopamine release and reward reinforcement |
| Withdrawal/Negative | Stress response and physical symptoms |
| Preoccupation | Craving activation and drug-seeking |
| External Triggers | Environmental cues and social pressures |
| Internal Triggers | Emotional states and learned associations |
This three-stage cycle creates a self-perpetuating loop where each phase strengthens the overall addiction pattern through distinct neural pathways and behavioral responses.
Evidence-Based Treatment Approaches
You’ll find robust evidence supporting a multi-modal approach to managing alcohol cravings through FDA-approved medications like naltrexone and acamprosate, which effectively reduce both physiological and psychological cravings when combined with behavioral therapies. Cognitive behavioral interventions, particularly exposure-response prevention and trigger-management protocols, demonstrate significant efficacy in restructuring your relationship with alcohol-related cues and developing adaptive coping mechanisms. Your success in managing stress responses can be maximized through evidence-based techniques such as mindfulness-based relapse prevention and biofeedback training, which show measurable reductions in cortisol levels and craving intensity.
Medication-Assisted Recovery Options
Medication-assisted treatment (MAT) offers evidence-based interventions for managing alcohol use disorder through FDA-approved medications that target specific neurobiological pathways. You’ll find that medication efficacy varies among the primary options, with acamprosate showing an NNT of 11 for relapse prevention and naltrexone demonstrating superior outcomes for heavy drinking reduction.
| Medication | Primary Action | Treatment Adherence |
|---|---|---|
| Acamprosate | Glutamate modulation | Daily dosing required |
| Naltrexone | Opioid receptor blockade | Oral or monthly injectable |
| Disulfiram | Acetaldehyde inhibition | Daily monitoring needed |
When combined with behavioral interventions, these medications greatly enhance treatment success rates. You’ll achieve ideal outcomes through personalized treatment plans that match your specific triggers and recovery goals, particularly when incorporating extended-release formulations to improve treatment adherence.
Cognitive Behavioral Intervention Strategies
Building upon pharmacological interventions, cognitive behavioral therapy (CBT) stands as a highly effective, evidence-based approach for treating alcohol use disorder. Digital CBT platforms like CBT4CBT have demonstrated over 50% increased abstinence rates compared to traditional methods across 8-month trials.
You’ll learn essential cognitive restructuring techniques to identify and modify distorted thinking patterns that fuel alcohol use. Through Socratic questioning and behavioral experiments, you’ll challenge beliefs about alcohol’s perceived benefits. The process includes developing personalized coping strategies to manage specific triggers, whether they’re emotional (anxiety, sadness), situational (social events, weekends), or environmental (locations, sensory cues).
Digital CBT platforms offer cost-effective, accessible solutions with interactive modules, progress tracking, and regular check-ins to reinforce your commitment to recovery and skill development.
Stress Response Management Techniques
While stress remains the predominant trigger for alcohol cravings, evidence-based stress response management techniques offer scientifically-validated pathways for recovery.
You’ll find that stress management through ACT and mindfulness-based interventions directly targets the neurological pathways that link emotional distress to alcohol seeking behaviors. These approaches strengthen your emotion regulation capabilities by teaching non-judgmental observation of difficult feelings without automatic substance use responses. Research shows that combining mindfulness meditation with cognitive-behavioral techniques helps you identify specific stressors while modifying maladaptive coping patterns.
When you integrate structured stress response protocols with physiological interventions targeting ghrelin signaling, you’re addressing both the psychological and hormonal components of cravings. This dual approach, supported by peer accountability systems, provides extensive tools for managing stress-induced urges through evidence-based mechanisms.
Frequently Asked Questions
How Long Does It Take for Alcohol Cravings to Completely Disappear?
Your craving duration varies considerably based on individual factors. While acute cravings peak within 72 hours, they’ll typically diminish over 1-2 weeks during clinical detox. However, you may experience protracted withdrawal symptoms for months. Craving triggers like stress, hormonal changes, and environmental cues can persist for years, though their intensity generally decreases over time. Complete neurochemical rebalancing of your brain usually takes several months to a year.
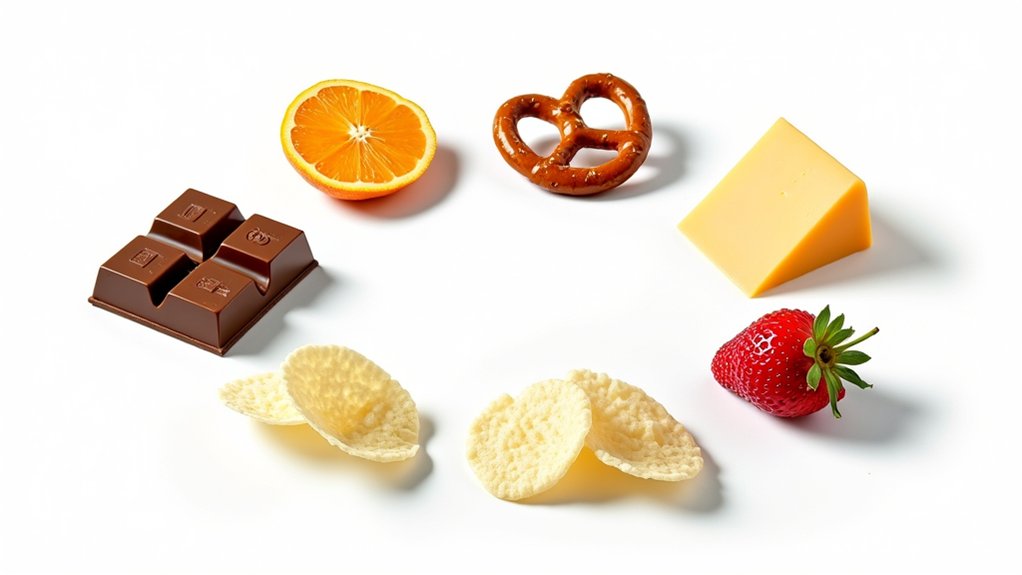
Can Certain Foods or Drinks Trigger Alcohol Cravings?
Yes, certain foods and drinks can trigger alcohol cravings through both biochemical and psychological mechanisms. Your brain creates food associations with past drinking experiences, making foods commonly consumed while drinking (like salty snacks or specific appetizers) potential triggers. Additionally, flavor similarities between non-alcoholic and alcoholic beverages can activate cravings – for example, the maltiness in non-alcoholic beer or the tannins in grape juice may remind you of their alcoholic counterparts.
Do Alcohol Cravings Get Worse With Age?
Research actually shows that alcohol cravings tend to decrease with age. You’ll likely experience reduced cravings as you get older due to aging effects on your brain’s reward systems. Clinical studies of 198 patients demonstrate significant reductions in craving intensity post-detoxification among older individuals. These changes stem from neurological changes in your mesolimbic pathways, where neurotransmitter efficiency naturally diminishes over time, leading to decreased craving responses.
Are Alcohol Cravings Stronger in Men or Women?
Research shows complex gender differences in craving intensity. While men tend to show hyperactive brain responses during cravings, women often experience more intense cravings triggered by stress and emotional factors. You’ll find that women typically develop stronger cravings with less alcohol consumption than men. Additionally, women’s cravings are more influenced by anxiety and social factors, while men’s cravings often relate to stress-specific neural pathways. The biological mechanisms driving these differences remain distinct between sexes.
Can Exercise Reduce the Intensity of Alcohol Cravings?
Yes, exercise can notably reduce alcohol craving intensity through multiple evidence-based mechanisms. You’ll find immediate benefits from both brief and extended exercise sessions. Research shows 12-minute aerobic workouts decrease cravings and negative mood states, while even 5-minute circuit training proves effective for craving management. Exercise’s benefits stem from improved stress regulation and mood enhancement, with studies demonstrating a one-third standard deviation reduction in craving intensity across various exercise types.